
Patient Information from ISHA – The Hip Preservation Society
Pigmented Villonodular Synovitis (PVNS)
Pigmented Villonodular Synovitis (PVNS)
Definition
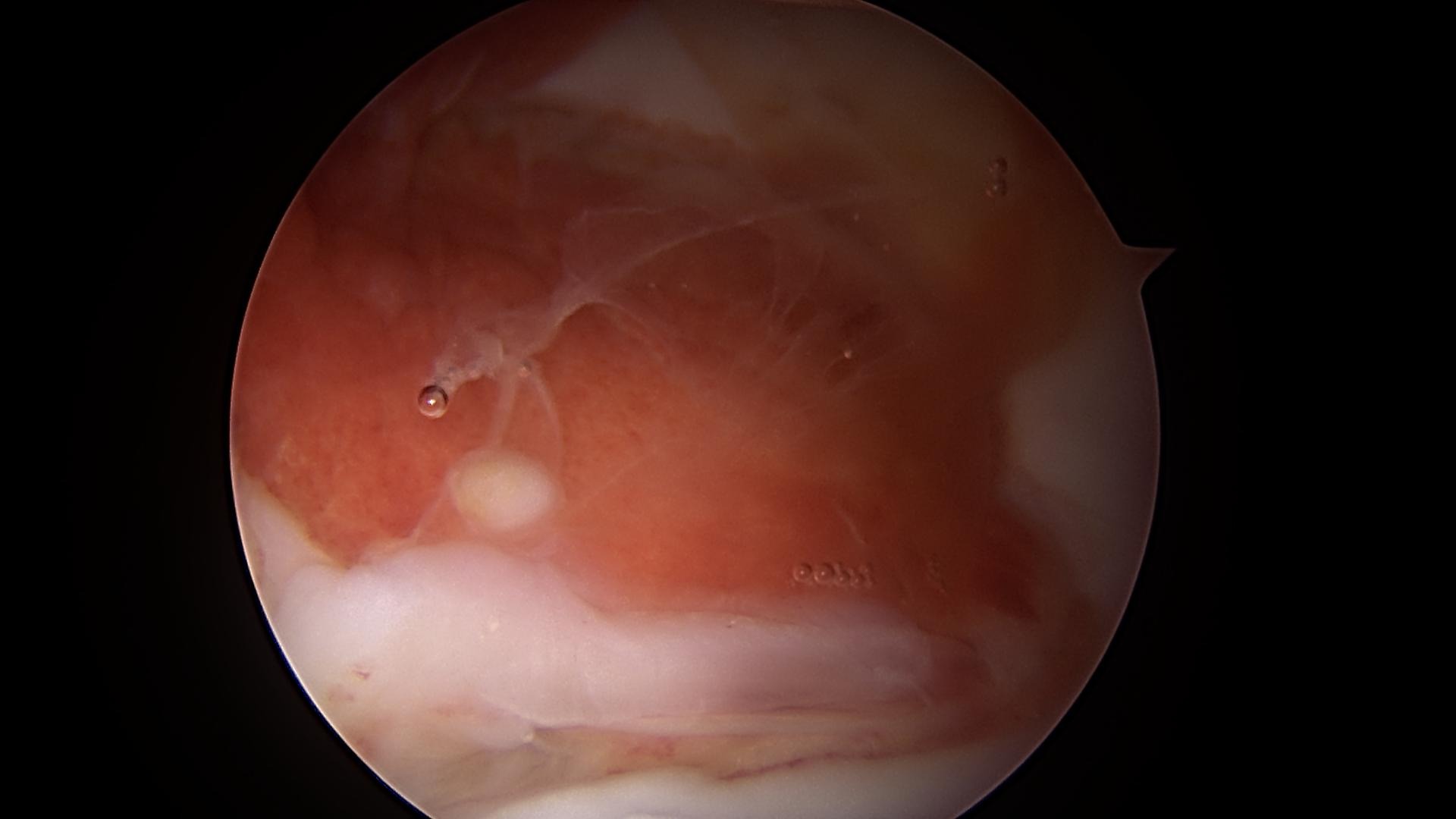
Pigmented Villonodular Synovitis (PVNS) is a benign (non-cancerous) condition affecting the joint lining (synovium). Its cause is unknown, it can affect any joint but is most seen in the knee.
It can also affect other soft tissues including tendon sheaths or bursaes. When it develops in the hip the joint lining becomes inflamed and thickened eventually causing damage to the articular surface of the joint if left untreated.
If the joint lining becomes severely deformed it may impact joint movement and function. In the hip it is more common in females and generally occurs between the ages of 30 and 50 years.
Signs and Symptoms
- Pain
- Reduced range of movement
Non-Surgical Treatment
- Radiation therapy may be used either in addition to surgery to lower the risk of recurrence but may also be used where previous surgery has been unsuccessful in managing widespread PVNS. Radiation side effects have to be considered before choosing this therapy.
- Drug injections including radiation injection therapy has proven helpful for some patients, but will come with side effects.
- New oral medications which are still being studied may be available depending on availability.
Surgical Treatment
Where the joint articular surfaces remain unaffected or are in good condition a synovectomy may be the treatment of choice. This involves removal of either part or all the joint lining – the extent of any damage will determine how much of the synovium is removed. Any synovectomy may be performed arthroscopically or via an open procedure using a larger incision. Conversely, if significant joint deterioration has occurred a total hip replacement may be the only treatment likely to relieve symptoms.
Even with surgery, the PVNS may recur and require additional treatments including repeat surgery or radiation therapy. There is a high recurrence rate of PVNS, specially with more aggressive presentations.

What to expect after surgery
Recovery following arthroscopic surgery is generally quicker than after an open procedure and hence returning to activities is also easier. Any return to sport will also depend on operative findings, and advice will be provided by the treating hip preservation surgeon and physiotherapist.
There may be limitations to weightbearing and activities during the first two or three months, which will vary amongst surgeons and will depend on operative findings and techniques performed.
Physiotherapy can begin after surgery, gradually increasing range of movement, stability, strength, mobility and function over a period of up to six months, depending on the surgery performed and individual aims.