
Patient Information from ISHA – The Hip Preservation Society
Femoroacetabular Impingement (FAI)
Femoroacetabular Impingement (FAI)
Definition
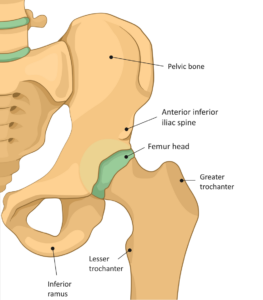
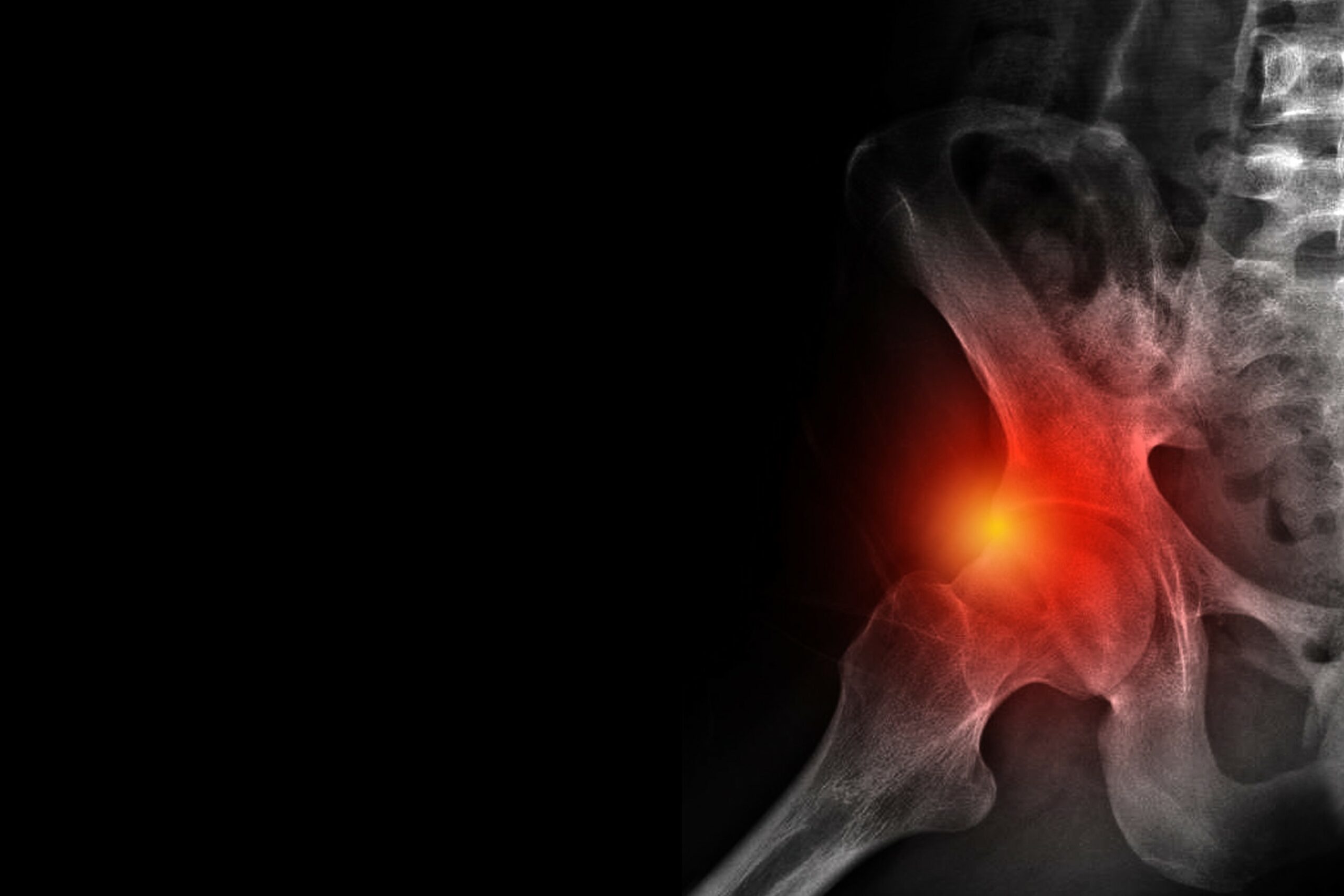
Femoroacetabular impingement (FAI) is characterised by overgrowth of bone on either the femoral head or the acetabulum (hip joint socket), resulting in reduced normal joint movement at the hip, which causes damage to the labrum and/or the articular cartilage.
FAI may develop:
- incidentally;
- as a result of the hip joint not developing normally during childhood;
- from activities requiring extremes of movement (e.g. dancing or gymnastics); or
- in the athletic population, when more vigorous movements are performed (e.g. soccer or hockey).
As the condition progresses, it may become more difficult to internally rotate the hip joint (turning ones toes inwards). To compensate for this loss of movement, symptoms in other areas may develop, including low back, groin, or gluteal pain. To overcome these difficulties, the gluteal muscles may overwork to protect the hip, which may result in discomfort and problems subsequently developing in this area too.
There are three types of FAI including Cam, Pincer and Combined impingement.
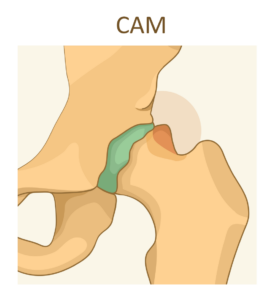
Cam
The femoral head is no longer rounded, with a bump forming on its edge at the junction with the femoral neck, which then rubs against the cartilage in the acetabulum during movement.
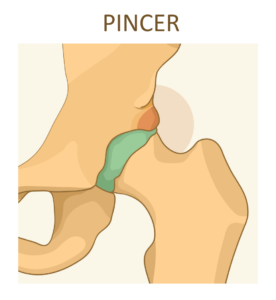
Pincer
Extra bone develops around the rim of the acetabulum.
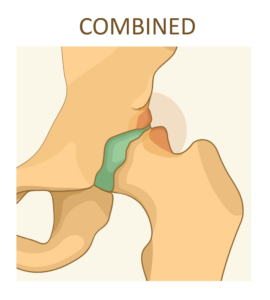
Combined
Both the pincer and cam types coexist in the same hip joint.
Signs and Symptoms
- Pain is often felt in the groin or outside of the thigh, but may also be present in the buttock, more diffusely around the thigh, lower back and knee
- Stiffness in the hip joint with associated loss of movement
- Limping resulting from an altered gait pattern
- Catching or clicking, which may occur if a labral tear has also developed
Diagnosis
A thorough physical examination may elicit pain suggestive of FAI, but imaging such as MRI and X-rays will be required to confirm or assist with a more formal diagnosis.
Non-Surgical Treatment
- Activity modification
- Use of anti-inflammatory medication
- Physiotherapy aiming to modify movement patterns by improving stability around the hip, pelvic and lumbar spine to ultimately help prevent the onset of pain during aggravating activities
Surgical Treatment
Aims of treatment are to reduce pain and improve function, as well as prevent or delay the onset of hip joint degeneration and osteoarthritis. Surgery may be arthroscopic or open, depending on the type of impingement and the location of other areas requiring attention. Treatment may include:
- Repair of labral tears, where often it is possible to stitch the labrum back onto the rim of the acetabulum, where it will heal well; any damage to the articular cartilage can also be “polished off” (chondroplasty)
- Removal of damaged or fraying cartilage, as well as any bone spurs to reduce friction during movement
- Removal of any loose pieces of cartilage or bone
- Osteoplasty – reshaping of the femoral neck or acetabulum
- Treatment to any areas of damaged cartilage using techniques such as microfracture
- Treatment to any surrounding soft tissues, which may include, but is not limited to, removal of inflamed bursaes, gluteal tendon repair, and removal of scar tissue (adhesions)
What to expect after surgery
Recovery following arthroscopic surgery is generally quicker than after an open procedure and hence returning to activities is also easier. There may be limitations to weightbearing during the first two or three months, which will vary amongst surgeons and will depend on what is found during surgery and the techniques performed. If microfracture is performed, partial weightbearing may be recommended for a longer period, when compared to just a labral repair, to allow tissue and bone healing to take place.
Physiotherapy can begin immediately after surgery, gradually increasing range of movement, stability, strength, mobility, and function over a period of up to six months, depending on the surgery performed and individual aims.